Sex differences in MS incidence and disease course suggest that hormonal regulation contributes to neuroimmune balance.
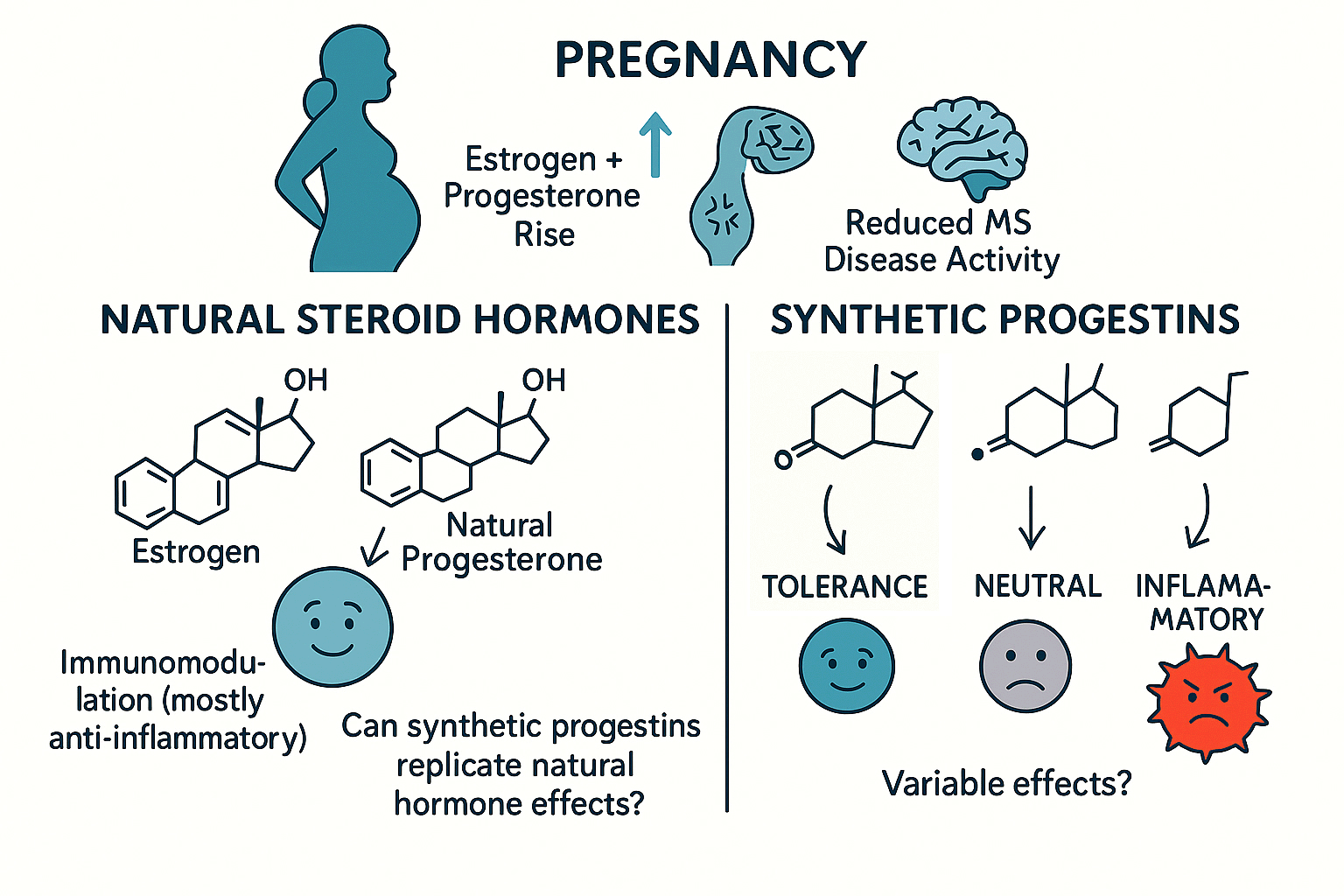
Progesterone promotes immune tolerance and tissue repair, yet many widely used synthetic progestins have distinct biological effects that are not equivalent to natural progesterone. Our research compares natural progesterone and multiple clinically used progestins using human PBMCs and the EAE model to determine how these hormones influence regulatory vs. pro-inflammatory immune responses, cytokine signaling, and neuroinflammation. This work aims to clarify which hormonal environments support immune homeostasis.
Key Findings & Interpretation
- Natural progesterone promotes immune-regulatory phenotypes, including increased Treg activity and reduced Th1/Th17 inflammatory responses.
- Several synthetic progestins do not replicate these effects and may have neutral or pro-inflammatory immune impacts depending on context.
- Progesterone and progestins differentially shape cytokine signaling, suggesting non-equivalence in neuroimmune outcomes.
- These results underscore the importance of distinguishing hormonal effects on immune pathways, rather than assuming all progestins act similarly.
Future Directions
- Use transcriptomic and receptor signaling analyses to define mechanisms by which progesterone promotes immune tolerance.
- Evaluate additional clinically relevant progestins in cellular and animal models to map their immune-regulatory profiles.
- Explore how hormonal context (e.g., pregnancy, postpartum, contraceptive use, menopause) interacts with microbial and immune pathways to influence disease activity in MS.